Benefits of breastfeeding
Benefits to your baby:
1. Breastmilk: a complete food
-
Breastmilk is meant to exactly suit the needs of your baby.
-
Breastmilk adapts to your baby’s changing nutritional needs as your baby gets older and has fewer feeds.
-
For around the first 6 months of life, your baby gets all the nutrients they need from breastmilk alone. Your baby will grow and develop well if you feed them only breastmilk and no solids, water or other liquids. This is called exclusive breastfeeding.
-
Breastmilk is easy to digest. It’s easily absorbed into your baby’s system.
2. Breastmilk: promotes healthy development
-
Colostrum is the first breastmilk that babies get when they’re born. Colostrum boosts your baby’s immune system and supports their growth and development.
-
Both colostrum and mature breastmilk have antibodies, good bacteria and other things that reduce your baby’s risk of infections like gastroenteritis, respiratory tract infections, ear infections and other problems like type-1 diabetes and type-2 diabetes, obesity and some cancers.
-
Breastmilk has fats and vitamins that are important for your baby’s brain development.
-
Breastfeeding is important for your baby’s eyesight, speech, jaw and mouth development.
-
Breastfed babies have a lower risk of sudden unexpected death in infancy (SUDI) including sudden infant death syndrome (SIDS) and fatal sleep accidents.
-
Breastmilk gives your baby a secure food source, even when power and clean water aren’t available.
-
Breastfeeding encourages skin-to-skin and eye contact between you and your baby. Being physically connected can help with bonding between you and your baby. This helps your baby feel secure and can help them form strong relationships as they grow up.
Benefits to mother:
1. Convenient
-
Breastfeeding is convenient and free. You don’t usually need special equipment to do it, and you can do it whenever and wherever you need to.
2. Weight loss
-
Breastfeeding can help some birthing mothers lose weight after birth.
3. Decreases risk of many illness
-
Women who breastfeed have lower rates of breast and ovarian cancer, osteoporosis, type-2 diabetes and high blood pressure. The longer you breastfeed, the better it is for your health.
When and how long to Breastfeed?
When to start breastfeeding?
-
World Health Organisation (WHO) recommends that breastfeeding should be initiated as soon as possible after birth, preferable within one hour of birth. This is crucial as the early skin to skin contact not only helps with bonding but also stimulates the baby's natural reflexes to suckel.
-
Colostrum, considered as Liquid Gold to the baby is produced in small quantities in first three days after birth. this Liquid Gold is packed with antibodies that help to protect newborn from various infection.
How long to breastfeed?
-
1. Exclusive Breastfeeding: The WHO recommends exclusive breastfeeding for the first six months of life. This means the infant receives only breast milk (and no additional foods or fluids, not even water) during this period. Exclusive breastfeeding provides optimal nutrition and supports healthy growth and development.
2. Continued Breastfeeding: After six months, it is advised to continue breastfeeding along with appropriate complementary foods. The WHO suggests breastfeeding should continue up to two years, depending on the mother and child’s preferences.
How to breastfeed?
Breastfeeding positions
1. Cradle Hold
-
The cradle hold is the most common position and helps provide an enjoyable feeding and bonding experience for both of you.
-
Sit somewhere with support to keep your arm at the right height, like an armed chair or couch. If needed, you can use pillows to support your arm.
-
Position your little one in your lap with their head in the crook of your arm.
-
Keep your baby’s chest against yours so they do not have to turn their head toward your breast. If necessary, use pillows to support your baby’s head.
2. Cross-cradle hold
-
This position is useful when first learning to breastfeed and is a great option for small babies. It allows you to have good control of your baby’s head while helping your little one to latch on.
-
Think of this as the reverse of the cradle hold. To perform the cross-cradle hold, position your baby in the opposite direction of the cradle hold with their head in your hand, rather than the crook of your arm.
3. Football Hold
-
If you are dealing with engorged breasts or sore nipples, this is a great position to try. This hold helps to prevent plugged ducts by positioning your baby to empty the bottom ducts – it's a win for both of you!
-
While turned on your side, hold your baby like a football or rugby ball along your forearm, with your baby’s body on your arm and face toward your breast.
-
Position your baby’s legs under your arm.
-
Use your other hand to support your breast.
-
The football hold is also helpful if you have undergone a Cesarean section and can’t place your baby on your stomach while nursing.
3. Side-lying Position
-
If you and your baby are more comfortable lying down, this is a great position to try.
-
Lay on your side and place your baby on their side, facing you, with their head at your breast.
-
Support your back with pillows and make sure that your baby’s nose isn’t obstructed.
-
This position is great for nighttime feedings and helps tired mothers relax while feeding.
4. Laid-back/ Reclining Position
-
If your little one has difficulty latching or is restless and crying, this is a calming position to try. In fact, this position is sometimes called “biological nurturing.”
-
Support yourself with pillows and lean far enough back for your baby to be fully supported on your reclined body – not completely flat.
-
Lay your baby prone on your chest. To engage in skin-to-skin contact, lay your naked baby on your bare chest and enjoy bonding with your little one.





Breastfeeding tips
1. Signs of a good latch
-
A comfortable experience with no pain.
-
More areola is visible above your baby’s mouth than below.
-
Your baby’s mouth is wide open.
-
Their lower lip is turned out.
-
Their chin is touching the breast.
2. Signs of poor latch
-
Baby's mouth is barely open.
-
Baby's lips are curled in.
-
Baby's chin is barely touching the breast.


3. Signs of good positioning
-
Your baby’s head and body are in line. A baby cannot suckle or swallow easily if their head is twisted or bent.
-
Your baby is held close to your body. A baby cannot attach well to the breast if they are far away from it.
-
Your baby’s whole body is supported with your arm along their back. This is particularly important for newborns and young babies.
-
For older babies, support of the upper part of body is usually enough.
-
Your baby approaches breast nose to nipple, so that they come to your breast from underneath the nipple.
4. Signs of effective suckling
-
Your baby takes slow deep suckles, sometimes pausing.
-
You may be able to see or hear your baby swallowing after one or two suckles.
-
Suckling is comfortable and pain free for you.
-
Your baby finishes the feed, releases the breast and looks contented and relaxed.
-
Your breast is softer after the feed.
Common breastfeeding problems
It is a myth that breastfeeding is easy. Breastfeeding takes time and practice for both mothers and babies. Many mothers experience challenges with breastfeeding, but the right support can help overcome these issues.
If you are facing issues with breastfeeding, reach out to your doctor or breastfeeding specialist or health care provider for support.
Here are some of the most common breastfeeding issues, and our tips that can help you find relief.
1. How do I make sure my baby has a good breastfeeding latch?
Establishing a proper latch is the key to making sure that breastfeeding is a comfortable experience for both you and your baby. To make sure your baby is well attached:
-
Bring their nose directly opposite your nipple.
-
Let their head tilt back a bit so their top lip can brush against your nipple. This should make their mouth open.
-
When their mouth is wide open, bring them quickly to the breast with their head back and chin leading. This way, your baby can take a large mouthful of breast and not just the nipple.
-
Your breast will be drawn deep into your baby’s mouth and your nipple will be positioned back into the soft part of your baby’s mouth. This will ensure you won’t get sore and your baby can get all the milk they need.
Signs of good attachment include:
-
A comfortable experience with no pain
-
More areola is visible above your baby’s mouth than below
-
Your baby’s mouth is wide open
-
Their lower lip is turned out
-
Their chin is touching – or nearly touching – your breast
2. What can I do about low milk supply?
It can be frustrating if you feel that you are not producing enough milk for your baby. If you are worried about your milk supply, reach out to your health care provider. In most cases, there is something going on that they will be able to help you identify.
Some common causes of low milk supply include:
-
A delay in initiating breastfeeding
-
No or very little skin-to-skin contact
-
A delay in milk coming in due to delivery complications, illness or diabetes
-
Poor attachment
-
Feeding at fixed times
-
Short feeds
-
No nighttime feeding
-
Infrequent feeds
-
Worry and stress
-
Lack of confidence
-
Lack of bonding
-
Dislike of breastfeeding
-
Tiredness
To help prevent low milk supply and maintain a healthy amount of breastmilk for your baby:
-
Engage in early skin-to-skin contact at delivery and initiate breastfeeding as soon as possible.
-
Ask for skilled breastfeeding support after delivery to ensure good attachment and effective suckling.
-
Practice rooming-in (staying and sleeping in the same room as your baby) 24 hours a day.
-
Breastfeed exclusively unless supplementing your milk supply is medically necessary as indicated by your health care provider.
3. What treatments are available for engorged breasts?
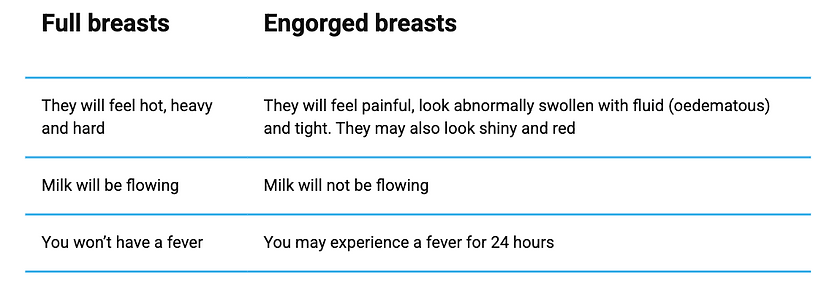
Having engorged breasts can be extremely painful. While full breasts can feel uncomfortable, engorgement is a different problem.
Common causes and ways to prevent engorged breasts include:
4. How can I prevent cracked nipples when breastfeeding?
Sore or cracked nipples are usually a sign that your baby is not properly attached at the breast when feeding. Make sure that your baby has a good latch. If one or both of your nipples begin to crack or bleed, reach out to your health care provider as soon as possible for support.
At home, try dabbing a bit of expressed breastmilk onto the nipples after you feed. Breastmilk has healing properties that help relieve soreness.
5. What causes mastitis and blocked milk ducts? How do I prevent them?
Breastmilk flows through a system of ducts in your breasts to reach your baby. Sometimes, an area of these ducts can become blocked which stops the milk from flowing easily. Blocked ducts can be painful.
Mastitis, an inflammation of the breast, can occur when a blocked duct does not clear or when the build-up of milk in your breast causes swelling or inflammation.
Speak to your breastfeeding consultant, or health care provider if you are experiencing pain from blocked ducts.
Some causes of blocked ducts and mastitis include:
-
Short or infrequent breastfeeds
-
Not removing the milk from part or all of the breast properly
-
Damaged breast tissue
-
Bacteria entering the breast through a crack in the nipple
To help relieve pain and treat your symptoms, try:
-
Improving milk removal
-
Correcting poor attachment
-
Wearing loose-fitting clothing
-
Breastfeeding more frequently
-
Gently massaging toward the nipple
-
Applying a warm compress to the area in pain
-
Varying feeding positions
Breastfeeding isn’t a ‘one woman’ job, and it is very common to run into bumps along the way. Reach out to your health care provider with any concerns and surround yourself with family, friends and loved ones for support along the way. You’ve got this!

Myths about breastfeeding
1. Myth: Breastfeeding is easy.
-
Babies are born with the reflex to look for their mother’s breast. However, many mothers need practical support with positioning their baby for breastfeeding and making sure their baby is correctly attached to the breast.
-
Breastfeeding takes time and practice for both mothers and babies.
-
Breastfeeding is also time intensive, so mothers need space and support at home and work.
2. Myth: It’s usual for breastfeeding to hurt – sore nipples are inevitable.
-
Many mothers experience discomfort in the first few days after birth when they are learning to breastfeed. But with the right support with positioning their baby for breastfeeding and making sure their baby is correctly attached to the breast, sore nipples can be avoided.
-
If a mother faces breastfeeding challenges like sore nipples, support from a lactation consultant or other skilled professional can help them overcome the issue.
3. Myth: You should wash your nipples before breastfeeding.
-
Washing your nipples before breastfeeding isn’t necessary.
-
When babies are born, they are already very familiar with their own mother’s smells and sounds. The nipples produce a substance that the baby smells and has ‘good bacteria’ that helps to build babies’ own healthy immune system for life.
4. Myth: You should separate a newborn and mother to let the mother rest.
-
Doctors, nurses encourage the practice of ‘skin-to-skin’ – also known as kangaroo mother care – immediately after birth.
-
Bringing your baby in direct contact, so their skin is against yours, is a very important practice that helps them to find and attach to the breast.
-
If you can practice this within one hour after birth and then frequently after, it helps to establish breastfeeding.
-
If the mother cannot do this, then the partner or another family member can step in.
5. Myth: You should only eat plain food while breastfeeding.
-
Like everybody else, breastfeeding mothers need to eat a balanced diet. In general, there is no need to change food habits.
-
Babies are exposed to their mothers’ food preferences from the time they are in the womb. If a mother perceives that her baby reacts to a specific food she eats, it is best to consult a specialist.
6. Myth: Exercise will affect the taste of your milk.
-
Exercise is healthy, also for breastfeeding mothers.
-
There is no evidence that it affects the taste of your milk.
7. Myth: You won’t be able to breastfeed unless you do it straight away.
-
It is easier to get breastfeeding started if you begin in the first hour after birth because a baby’s reflexes are very strong at that time. They are ready to learn to feed at the breast.
-
If you do not latch your baby on right after birth, do it as soon as possible in your situation.
-
If you need help putting your baby to the breast, ask for support from a qualified lactation consultant or other skilled professional.
-
Frequent skin-to-skin contact and putting your baby to the breast will help to get breastfeeding going.
8. Myth: You can never use formula if you want to breastfeed.
-
Mothers may decide they need to use formula on some occasions, while continuing to breastfeed.
-
It is important to seek unbiased information on formula and other products that replace breastmilk.
-
To keep breastmilk production going, continue offering the breast to your baby as often as possible.
-
It can be useful for mothers to consult a lactation specialist or skilled professional to help with a plan that works best for them to continue breastfeeding.
9. Myth: Many mothers can’t produce enough milk.
-
Almost all mothers produce the right amount of milk for their babies.
-
Breastmilk production is determined by how well the baby is latched on to the breast, the frequency of breastfeeding and how well the baby is removing milk with each feeding. Breastfeeding isn’t a ‘one woman’ job and mothers need support.
-
Support like ongoing breastfeeding guidance from health care providers, help at home, and staying healthy by eating and drinking well.
10. Myth: You shouldn't breastfeed if you’re sick.
-
Depending on the kind of illness, mothers can usually continue breastfeeding when they’re sick.
-
You need to make sure you get the right treatment, and to rest, eat and drink well.
-
In many cases, the antibodies your body makes to treat your disease or illness will pass on to your baby, building their own defences.
11. Myth: You can’t take any medication if you’re breastfeeding.
-
It’s important to inform your doctor that you are breastfeeding and to read the instructions with any medications you buy over the counter.
-
It might be necessary to take medications at a specific time or in a specific dosage, or to take an alternative formulation.
-
You should also tell the baby’s doctor about any medications that you’re taking.
12. Myth: It’s hard to wean a baby if you breastfeed for more than a year.
-
There’s no evidence that it is more difficult to stop breastfeeding after one year, but there is evidence that breastfeeding up to two years is beneficial for both mothers and children.
-
All mothers and babies are different and need to determine together how long they want to breastfeed.
13. Myth: If you go back to work, you’ll have to wean your baby.
-
Many mothers continue breastfeeding after going back to work.
-
First, check the policies in your own workplace.
-
If you have the right to time and a place to breastfeed during working hours, you may be able to go home and breastfeed, ask a family member or friend to bring your baby to you, or to express your milk and take it home.
-
If you don’t have the option to breastfeed during working hours, look for moments during the day to express your milk and then feed your baby directly when you are at home. If you decide to give your baby a breastmilk substitute for some feeds, it still very good to continue breastfeeding whenever you are with your baby.
